Main Second Level Navigation
- Bachelor of Science in Medical Radiation Sciences
- Medical Physics Residency
- Radiation Oncology Residency
- Radiation Oncology Fellowship
- Visiting and Elective Residents and Fellows
- Clinical and Experimental Radiobiology Course
- MR-integrated Radiation Therapy Training Program
- Learner Mistreatment
- Electives and Observerships
- MSc and PhD
- Student Life and Resources
- STARS21
- Teaching Evaluations
Breadcrumbs
Radiation Therapy
Radiation therapy is the treatment of cancer and other diseases using radiation. In high doses, radiation kills cells or keeps them from growing and dividing. Because cancer cells grow and divide more rapidly than most of the normal cells around them, radiation therapy can successfully treat many kinds of cancer.
Radiation Therapy can be delivered in different ways. External beam radiotherapy uses machines to focus radiation on a cancer site. Depending on the radiation beam energy, it can be used to destroy cancer cells both on the surface and deeper in the body. The higher the energy of the beam, the deeper the radiation can penetrate into the target tissue.
Internal radiotherapy, or brachytherapy, places radioactive implants directly in a tumour or body cavity. In this treatment, the radiation dose is concentrated in a small very area.
What does a Radiation Therapist do?
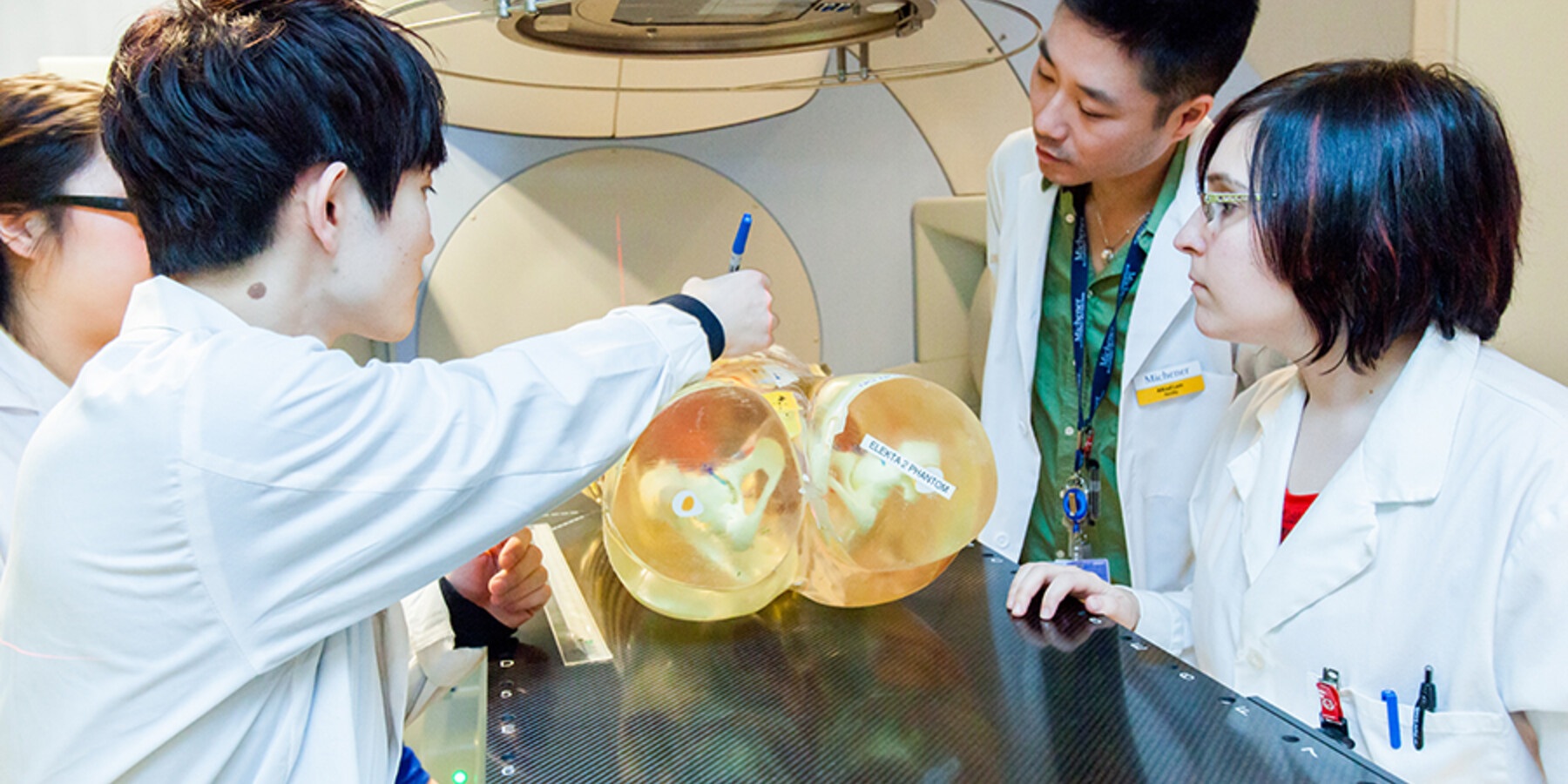
Working closely with doctors, medical physicists, patients and other members of the health care team, Radiation Therapists navigate highly technical equipment while delivering empathetic and patient-centered care. Radiation Therapists use advanced computer systems and radiation therapy equipment to design and implement treatment plans and deliver radiation treatment, including:
- Planning all treatment details, including calculating the radiation dose and simulating its distribution
- Positioning the patient and operating the radiation therapy equipment
- Constructing and fitting accessory devices that shape, modify and direct the radiation to destroy cancerous tissue
- Therapists also play an important role in counseling patients on possible side effects from treatments and provide advice on how best to minimize these effects. Because radiation treatments often extend over several weeks, a special supportive relationship often develops between the therapist, the patient and the patient’s family.
Is Radiation Therapy a good choice for you?
Radiation Therapists are detail-oriented and enjoy applying their knowledge of biology, mathematics and physics, since their work requires precision and the safe operation of sophisticated equipment. In addition to employing technical expertise in computerized systems used to for the simulation and planning of treatment details, Radiation Therapists provide the patient and their family with in-depth and continuous care, support, and counseling throughout the treatment process. Although future career opportunities may take you into other work environments, Radiation Therapists are typically employed in Cancer Centres and work with their patients during scheduled appointments over weeks or several months.
Future career opportunities as a Radiation Therapist include research activities, advanced roles such as the clinical specialist radiation therapist (CSRT), management, education, sales/marketing, other specialties such as magnetic resonance imaging (MRI) and computed tomography (CT), higher education at a master’s level, and working abroad.
Graduates of the Radiation Therapy stream of the MRS program will earn a BSc in Medical Radiation Sciences from the University of Toronto and an Advanced Diploma in Health Sciences (Radiation Therapy) from The Michener Institute. MRS graduates are eligible to write the national certification exam offered by the Canadian Association of Medical Radiation Technologists (CAMRT) and may pursue advanced studies at U of T or Michener, such as:
- Magnetic Resonance Imaging (MRI)
- Master of Applied Science (Institute of Medical Sciences)
- Master of Health Administration
MRS Clinical Placements - Radiation Therapy
Radiation Therapy students gain experience through non-paid clinical placements at one or more sites across Ontario including sites in Mississauga, Newmarket, Barrie, Ottawa, Kingston, Oshawa, Sudbury, Thunder Bay, Windsor and Toronto*. There are also out-of-province opportunities** in New Brunswick, Newfoundland and Nova Scotia. (see below). Radiation Therapy students graduate with 42 weeks of clinical experience:
- 8 weeks at the end of Year 1
- 4 weeks at the end of Year 2
- 30 weeks in Year 3
*Please note that placement at your first-choice site is not guaranteed and that clinical site locations are subject to change.
Out-of-Province Opportunities**
Radiation Therapy applicants who wish to explore their career outside of Ontario may be eligible for the following MRS Out-of-Province Opportunities:
- New Brunswick - Saint John School of Radiation Therapy, Horizon Health Network
- Newfoundland and Labrador Health Services (NLHS) - Provincial Cancer Care Program
- Nova Scotia - Cancer Care Program, Nova Scotia Health Authority
**Please note that your eligibility for these Out-of-Province opportunities are subject to terms and conditions set by the sponsoring agency.
MRS Course List* - Radiation Therapy
*Subject to Change
YEAR 1 FALL – SEMESTER 1
MRS142H1 / RSRT310 – Introduction to Radiation Physics
The interactions of ionizing radiation with matter occur in the subatomic realm, and are well described by the principles of basic radiation physics. These interactions set off a complex chain of biochemical and biological events at the atomic, molecular, and tissue/organ level that may result in biological damage. This course examines the different types of radiation and how they interact with matter. Pertinent properties of both the radiation and the materials that dictate the nature of the interaction are discussed. A review of the structure of matter also reveals the physical origin of radiation production in relation to both external radiation therapy and brachytherapy. Based on the understanding of radiation interactions with matter, radiation units and methods of radiation dosimetry are described. Finally, the principles of operation of radiation therapy machines and the importance of quality assurance procedures in the radiation therapy department are discussed.
MRS143H1 / RBRT310 – Radiobiology & Radiation Protection
After a brief overview of the course and an introduction to the nature of cancer, aspects of the physics and chemistry of ionizing radiation will be discussed. The cellular and molecular effects of ionizing radiation and how they help in the understanding and current practice of radiation therapy will form the major emphasis of the course. The effects of whole body exposure to ionizing radiation at a somatic, teratogenic and genetic level will be studied. Sources of data on the effects of human exposures to ionizing radiation will be described. From this data it will be shown how the risks associated with exposure to ionizing radiation have been determined. National and international standards regarding acceptable exposure levels and the Canadian legislation and regulatory bodies that deal with ionizing radiation will be discussed. There will be a description of a typical radiation protection program at a radiation therapy facility. This section will detail the administrative requirements of the program, radiation shielding design, procedures for staff and patient exposure reduction and personnel monitoring. Sources of radiation in a typical radiation therapy facility will be described and the exposures typically received by staff will be discussed. To help illustrate these radiation protection concepts there will be a laboratory held at a radiation therapy facility.
MRS159H1 / ANAT110 – Anatomy for Medical Radiation Sciences
This is an online course and is designed to serve as a foundation in Human Anatomy for students in the Medical Radiation Sciences (MRS) program. The course is a 0.5 academic credit and will introduce students to the components of the human body, relationships of the surface anatomy and the body's internal components and discuss the basic function of these components. The course will encompass a regional approach to study the human body with correlation to its clinical application. ANRD111 precedes Human Physiology (PSRD120/MRS162H1). It provides the students with an anatomical background prior to learning the regional and systematic functions addressed in the Physiology course. Anatomy for MRS will also serve to prepare students for ANRD121/ MRS164H1 (Relational Anatomy).
MRS227H1 / PMRS111 – Patient Care in Medical Radiation Sciences I
This course forms the foundations of patient care management for students in the University of Toronto/Michener Institute Medical Radiation Sciences Program. Learners are provided with the opportunity to learn about and practice the common technical and non-technical skills necessary for caring for patients in the clinical environment. Topics covered in this course range from reflective practice and journaling to vital signs assessment and infection control. The topics included in this course will provide essential as the learner progresses through both the didactic and clinical components of the Medical Radiation Sciences Program.
MRS281H1 / IGRD110 – Comparative Medical Imaging
This course is designed to introduce the learner to the complexities of diagnostic and therapeutic imaging in the healthcare setting. Learners will develop an understanding of what it means to be a medical radiation technologist, a healthcare professional, and to the concept of professionalism. As well, learners will be exposed through a series of seminars delivered by healthcare professionals from the practice setting, to a variety of imaging modalities used in the diagnosis and treatment of patients. Modalities such as X-ray, Computed Tomography (CT), Magnetic Resonance Imaging (MRI), Ultrasound (US), Positron Emissions Tomography (PET), and Image Guidance for Radiation Therapy will be studied. Additional topics relating to the imaging modalities that will be covered are image fusion, radiation safety and dose reduction. In addition, a structured interprofessional education session will be scheduled to explore professionalism in the context of collaboration and communication with other health profession students.
MRS144H1 / ONRT120 – Introduction to Clinical Oncology
This course provides the student with an understanding of the concepts of oncology, including epidemiology and etiology, clinical signs and symptoms, routes of spread, pathology, staging systems and the principles of treatment for the primary modalities utilized in the management of cancer. Topics covered include: diagnostic and staging workup, prognostic factors, the therapeutic decision-making process, and treatment outcomes. In addition, students will be introduced to basic radiographic principles in order to provide the necessary foundation material for further imaging studies.
YEAR 1 WINTER – SEMESTER 2
MRS145H1 / RSRT320 – Radiation Beams and Their Interactions
In the majority of radiation therapy treatments, external radiation beams are used to deliver a prescribed radiation dose to a predetermined tissue volume (target volume) while the dose outside this volume must be kept to an acceptable minimum. To accomplish this, a suitable number and arrangement of desirable beams will be added together to produce a treatment plan. The relative doses at various locations are calculated from the predetermined radiation beam data to assess the suitability of the treatment plan. The first part of this course covers the methods of characterising radiation beams in air and in a standard phantom. Relevant beam data (PSF (peak scatter factor), %DD (percent depth dose), TAR (tissue air ratio), TPR (tissue phantom ratio), and their dependence with beam energy, treatment distance and other parameters are described. Clinical applications of this data in patient dose calculations are illustrated using a number of basic external beam therapy techniques.
MRS228H1 / PMRS121 – Patient Care in Medical Radiation Sciences II
In this course, learners will build upon the knowledge acquired in PMRS111 as they apply the concepts of professional practice, patient management and health and safety, in both the didactic and laboratory environments. Learners will employ principles of infection control, patient assessment, patient transfer, contrast media administration and emergency response procedures. Learners will also be introduced to various venipuncture techniques. These practical skillsets will be developed as learners simultaneously integrate the concepts of patient-centred communication and professionalism introduced in PMRS111.
MRS155H1 / RTRT120 – Radiation Therapy Methodology I
The course will introduce the learner to the radiation therapy treatment delivery process. The learner will develop psychomotor and problem-solving skills that will be utilized for application of radiotherapy treatment. The learner will have the opportunity to practice technical and client communication, interpreting documentation, image acquisition and assessment, quality assurance procedures, setup, and safety.
MRS164H1 / ANRD121 – Relational Anatomy
For the purposes of diagnosis and optimal treatment of abnormal patient conditions, high quality, detailed images are required in order to obtain information on the anatomical state of an organ or structure within the body. The ability to recognize anatomical structures as demonstrated on CT or MR images in sagittal, coronal and axial sectional planes is essential in the current hospital imaging environment. The Relational Anatomy course investigates gross, cross-sectional and relational anatomy of the head, central nervous system, neck, spine, thorax, abdomen, male / female pelvis, upper / lower extremities. An emphasis is placed upon the organs, the vascular system, the lymphatics system as well as muscular and skeletal structures. This course offers weekly interactive lectures and labs which provide the student with a stimulating environment in which they may actively apply the knowledge learned through the use of a variety of media including anatomical models, preserved human specimens, cadaver cross section images as well as a multitude of hard copy and computer based medical images.
MRS162H1 / PSRD120 – Physiology
This course is an introductory ONLINE course designed to serve as the foundation in Human Physiology for students in the Medical Radiation Science program. It is intended for students who have an interest in or a need for a basic course in Human Physiology. The course is a 0.5 credit course and will introduce students to the function of the organ systems that comprise the human body. The course will follow a systematic structure covering all of the principal functional systems within the body, such as the cardiovascular and respiratory systems. As such students are expected to be familiar with the anatomical structure of these systems. Clinical examples will be used to illustrate key principles and material where possible.
YEAR 1 SUMMER – SEMESTER 3
MRS156H1 / CLRT130 – Introduction to Clinical Radiation Therapy
CLRT130 Introduction to Clinical Radiation Therapy is an 8-week course during which students apply the knowledge, behaviours, and skills gained through the previous two semesters. Through a combination of simulated clinical activities and clinical hospital-based rotations, the student will familiarize themselves with their future roles as Radiation Therapists as well as gain an enhanced understanding of the significance of collaborative patient-centred care and an understanding of the cancer patient experience.
Selective I
The specialized electives (“selectives”) are courses developed with the purpose of providing graduates of the Medical Radiation Sciences (MRS) Program with knowledge and expertise in specialized fields of practice. Selectives are designed to give students some freedom in constructing a curriculum that responds to their own particular interests related to their chosen profession and/or academic endeavors after graduating from the program.
Examples of selective courses that are available to MRS students are: MRI, Informatics, Introduction to Brachytherapy, Patient Education, Supportive and Palliative Care, and many more.
YEAR 2 FALL – SEMESTER 4
MRS146H1 / ONRT410 – Clinical Oncology I
The intent of this course is for the student to relate the core principles of clinical oncology to a diverse spectrum of clinical cases. These principles address issues along the entire spectrum of the clinical course of cancer, and focus primarily on issues that affect the individual patient rather than on population health. The course will also provide an overview of current areas of research and controversy in the clinical management of cancer.
MRS158H1 / RTRT240 – Radiation Therapy Methodology II
The course will build on the skills developed in Methodology in Radiation Therapy I, anatomy, oncology and treatment planning. The course is designed to foster critical thinking and problem-solving skills that a student requires to participate in simulator planning and treatment delivery processes. Laboratories will include conventional simulation, virtual simulation, and resimulation along with image assessment and archiving.
MRS244H1 / RSRT231 – Treatment Planning I
The purpose of this course is to build on the fundamentals of radiation physics and to develop dosimetric problem solving skills through the application of theory to clinical situations. Topics will include: planning methods for photon and electron beams, beam modifications for patient data and dose calculations. In addition to the topics covered in the lecture series, students will have an opportunity to reinforce and demonstrate the principles of radiotherapy treatment planning by creating and assessing isodose distributions for various clinical scenarios.
MRS257H1 / RTIM240 – Imaging in Radiation Therapy
Imaging in Radiation Therapy is an introductory course for students in the Radiation Therapy program. The course familiarizes the students with techniques in CT simulation, as well as expands on emerging imaging being used in the discipline, including MR simulation, PET, CBCT, US and Diagnostic CT. Students will develop hands-on skills pertaining to simulation in radiation therapy. Using a phantom, the learners will participate in simulated clinical applications of computed tomography simulation of common sites for treatment with radiation therapy with a focus on patient position, accurate documentation, dose management and optimization. Registration of datasets with those of other modalities used in clinical treatment planning practice will also be explored. This course consists of 2.5 hours of lecture and 2 hours of lab per week.
MRS266H1 / RMIP240 – Introduction to Research Methods
This course provides an introduction to research methods and designs relevant to practitioners of the medical radiation sciences. This course will focus on an introduction to various research designs including experimental and non-experimental, and quantitative and qualitative research methods. In addition, the course will focus on providing a practical understanding of several basic statistical tools used in medical and health research.
MRS260H1Y / EMRS240 – Experiential Learning in IPEC
"lnterprofessional education (IPE) occurs when students from two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes" (WHO, 2010). At the academic level, the goal of IPE is to prepare health professional students with the knowledge, skills and attitudes necessary for collaborative interprofessional practice (http://ipe.utoronto.ca/).
Experiential Learning in lnterprofessional Education and Collaboration is a longitudinal, two semesters, course consisting of online asynchronous and synchronous learning activities. Online asynchronous self-directed activities will explore and examine key concepts and skills surrounding IPE, reflection, and communication.
Synchronous experiential learning activities will expose students to other health profession students in various contexts to enable them to better understand health profession roles, appreciate team dynamics in healthcare, and learn with and from each other. Through the various learning opportunities, MRS students will gain valuable collaborate and communication skills to help prepare them to be collaborative practice-ready healthcare professionals. This course is interactive and requires full participation. Students will be required to reflect on course content and activities and prepare a longitudinal portfolio that reflects the values and competencies of interprofessional education and collaboration.
YEAR 2 WINTER – SEMESTER 5
MRS150H1 / ONRT420 – Clinical Oncology II
The intent of this course is for the student to relate the core principles of clinical oncology to a diverse spectrum of clinical cases. These principles address issues along the entire spectrum of the clinical course of cancer, and focus primarily on issues that affect the individual patient rather than on population health. The course will also provide an overview of current areas of research and controversy in the clinical management of cancer.
MRS160H1 / RTRT250 – Radiation Therapy Methodology III
Through opportunities for integration and application of the learner's knowledge of anatomy, oncology, physics and treatment planning, the student will be able to justify or appraise the choice of treatment and simulator techniques for complex sites. The learner will have the opportunity to perform CT and MR simulation in laboratories. The learner will incorporate aspects of patient care and communication into all procedures.
MRS245H1 / RSRT241 – Treatment Planning II
This course builds on the fundamentals of classic dosimetry covered in RSRT231 by introducing the learner to the principles of treatment planning in the modern era. The course begins with a primer in Brachytherapy and then moves on to modern external beam planning through investigation of the various the image modalities used in treatment planning and by covering the fundamentals of 3D conformal radiation therapy and intensity modulated radiation therapy. In addition to the topics covered in the lecture series, students will have an opportunity to reinforce and demonstrate the principles of modern radiotherapy treatment planning by creating and assessing isodose distributions for various clinical scenarios.
MRS269H1 / HBRD241 – Clinical Behavioural Sciences
This course provides an overview of the ethical, societal and personal factors that influence and impact health care services. The role of the health care provider and the dynamics of the provider/patient relationship will be examined from a critical perspective. Through an interprofessional education session students will explore alternate models of healthcare provision. This course will combine theory and practical application, allowing the student to reflect on his or her own values and beliefs through case studies, reading and discussion.
MRS229H1 / PCRT250 – Patient Care in Radiation Therapy
This course builds upon the foundational knowledge and skills gained from Patient Care in Medical Radiation Sciences I and II by addressing the care needs of oncology patients undergoing radiation therapy treatment for a variety of disease sites. Emphasis is placed on assessment, intervention, and patient care skills specific to the practice of radiation therapy. The course covers the basic principles of pharmacologic interventions, nutrition, and palliation. Labs with emphasize communication, assessment, and client education skills with the use of role playing exercises and evaluations. Case studies will be utilized to provide learners with the opportunity to integrate patient care communication and technical skills.
MRS260H1Y / EMRS240 – Experiential Learning in IPEC (Continued)
"lnterprofessional education (IPE) occurs when students from two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes" (WHO, 2010). At the academic level, the goal of IPE is to prepare health professional students with the knowledge, skills and attitudes necessary for collaborative interprofessional practice (http://ipe.utoronto.ca/).
Experiential Learning in lnterprofessional Education and Collaboration is a longitudinal, two semesters, course consisting of online asynchronous and synchronous learning activities. Online asynchronous self-directed activities will explore and examine key concepts and skills surrounding IPE, reflection, and communication.
Synchronous experiential learning activities will expose students to other health profession students in various contexts to enable them to better understand health profession roles, appreciate team dynamics in healthcare, and learn with and from each other. Through the various learning opportunities, MRS students will gain valuable collaborate and communication skills to help prepare them to be collaborative practice-ready healthcare professionals. This course is interactive and requires full participation. Students will be required to reflect on course content and activities and prepare a longitudinal portfolio that reflects the values and competencies of interprofessional education and collaboration.
YEAR 2 SUMMER – SEMESTER 6
MRS232H1 / HIRT130 – Health Improvement Initiatives
Health Improvement Initiatives is a 12-week summer semester course that will focus on the intersection of three principle domains of healthcare system, leadership, quality. The course will explore the organization and structure of the Canadian healthcare system to better understand and appreciate the roles and accountabilities of those who use and those who function within it. It will also examine healthcare leadership at all levels and the practitioner needed for today’s dynamic healthcare environment. Lastly, the course will focus on understanding quality improvement initiatives aimed to make healthcare more effective, efficient, and safe.
MRS241H1 / CLRT261 – Simulated Clinical Experience: Radiation Therapy
This course is designed to prepare the learner for entry into the clinical component of the radiation therapy program. The learner will have the opportunity to integrate and apply his/her knowledge, skills, and behaviours to various radiotherapy case scenarios through the use of clinical simulation. Ultimately the learner must demonstrate the requisite level of performance in order to proceed into the clinical environment.
MRS230H1 / TCRT266 – Transition to Clinical Radiation Therapy
This transition course has been designed to provide students with opportunity to familiarize themselves with the site, further enhance their knowledge, skills and judgement from the didactic and clinical simulation (CLRT261/MRS241HI) environments. As they transition into radiation therapy practice and subsequently the Clinical Practicum II and III, the primary focus of the students’ experience will be on interacting with the interprofessional team, providing patient-focused care, and demonstrating safe practice in the clinical environment.
During this course, the student is expected to integrate the patient care, communication and basic radiation therapy technical skills learned, into the practice of radiation therapy. The student is expected to reflect on their practice and integrate external feedback received, in order to identify learning goals that help them to improve and be successful as they progress to the next clinical course.
While the learner is expected to successfully complete the course objectives outlined later in this document, he/she is not restricted to these tasks. The student and the Clinical Coordinator at each clinical site will discuss and mutually agree upon any additional learning activities / objectives / or competencies not explicitly outlined in this document.
Attendance is mandatory, for any time off or illness, the student is expected to follow the clinical site procedure and the policies outlined in the MRS handbook. The student may be requested to submit a verification of illness form upon their return due to illness.
Selective II
The specialized electives (“selectives”) are courses developed with the purpose of providing graduates of the Medical Radiation Sciences (MRS) Program with knowledge and expertise in specialized fields of practice. Selectives are designed to give students some freedom in constructing a curriculum that responds to their own particular interests related to their chosen profession and/or academic endeavors after graduating from the program.
Examples of selective courses that are available to MRS students are: MRI, Informatics, Introduction to Brachytherapy, Patient Education, Supportive and Palliative Care, and many more.
YEAR 3 FALL – SEMESTER 7
MRS242H1 / CLRT371 – Clinical Radiation Therapy II
This clinical course provides the student with further opportunity to develop the skills and behaviours practiced in CLRT130 and the simulation semester. The student will be provided with a wide variety of experiences that encourage the integration and application of their didactic knowledge in the clinical setting. The student in this course will begin to develop competence in Radiation therapy as outlined in the CAMRT Competency Profile and Summary of Clinical Competence. Staff professionals and Clinical Coordinators work with the student to facilitate the achievement of these goals.
RMRD370 / MRS398Y1 – Research Methods
This two-semester course is the practical component of the Introduction to Research Methods course (MRS265H1/RMIP240). It allows for the completion of a clinically based research project under supervision. The research question and subsequent project may be pre-determined by the clinical research supervisor as it will most likely pertain to the supervisors' research area of interest and clinical expertise. Students will be matched with a research supervisor at their clinical host site to facilitate the development of a clinically relevant and feasible research study.
Delivery and support of this course is principally on-line and at a distance. However, students may be required to present assignments in-person or via live-electronic media in the winter semester of the course. The opportunity to meet in-person or on-line will assist in establishing a collegial research network and community amongst the learners. Completion of the research project will culminate in the submission of a written research thesis. Students will be encouraged to complete work of publishable quality.
This course is recommended for students who are interested in pursuing graduate studies and/or an academic career in Medical Radiation Sciences
- OR -
MRS397H1 / RPRD370 – Research in Practice
Research in Practice is a one semester online course designed to provide an opportunity for learners to critically examine the role that research plays in informing and advancing practice. Through an inquiring examination of clinical practice, the learner will gain an appreciation for evidence-based practice and research. The course consists of independent self-directed assignments in which the learner will review and critically appraise a procedure/guideline from practice (imaging, therapeutic, patient, safety), generate questions and rationale for further investigation, and conduct a search of current literature that leads to a written review of evidence-based practice.
YEAR 3 WINTER – SEMESTER 8
MRS243H1 / CLRT380 – Clinical Radiation Therapy III
This is the final clinical course. It provides the student with the final opportunity to develop the skills and behaviours practiced in CLRT371/ MRS242H1. The student will be provided with a wide variety of experiences in the clinical setting, in all professional behaviour situations, they are expected to meet the expectations of an entry level practitioner. The student in this course is expected to demonstrate competence in all the required skills as outlined in the CAMRT Competency Profile and Summary of Clinical Competence. Staff professionals and Clinical Coordinators work with the student to facilitate the achievement of these goals as they approach the end of their clinical experience. Supervision of the student may be by direct or indirect observation, at the discretion of the presiding clinical Coordinator or clinical staff.
RMRD370 / MRS398Y1 – Research Methods (Continued)
This two-semester course is the practical component of the Introduction to Research Methods course (MRS265H1/RMIP240). It allows for the completion of a clinically based research project under supervision. The research question and subsequent project may be pre-determined by the clinical research supervisor as it will most likely pertain to the supervisors' research area of interest and clinical expertise. Students will be matched with a research supervisor at their clinical host site to facilitate the development of a clinically relevant and feasible research study.
Delivery and support of this course is principally on-line and at a distance. However, students may be required to present assignments in-person or via live-electronic media in the winter semester of the course. The opportunity to meet in-person or on-line will assist in establishing a collegial research network and community amongst the learners. Completion of the research project will culminate in the submission of a written research thesis. Students will be encouraged to complete work of publishable quality.
This course is recommended for students who are interested in pursuing graduate studies and/or an academic career in Medical Radiation Sciences
- OR -
Selective III
The specialized electives (“selectives”) are courses developed with the purpose of providing graduates of the Medical Radiation Sciences (MRS) Program with knowledge and expertise in specialized fields of practice. Selectives are designed to give students some freedom in constructing a curriculum that responds to their own particular interests related to their chosen profession and/or academic endeavors after graduating from the program.
Examples of selective courses that are available to MRS students are: MRI, Informatics, Introduction to Brachytherapy, Patient Education, Supportive and Palliative Care, and many more.