Personalized Cancer Medicine and Adaptive Radiotherapy
THIS IS AN EXCERPT FROM THE 2016-2017 ANNUAL REPORT.
Contributors: Claire McCann, Tim Craig, Arjun Sahgal, Brian Keller
Personalized Cancer Medicine (PCM) also known as precision medicine has defined a new era in oncology with the recognition that tumors once classified solely by their tissue of origin in fact consist of multiple genetically distinct subgroups, and as such, the ability to categorize tumors into smaller subgroups defined by molecular makeup would have an important impact on treatment design, approach and modality.
The concept of one treatment for one tumour tissue type no longer applies, as molecular abnormalities specific to the tumour subgroup can be targeted by specific drugs or treatments such as molecularly targeted therapies and/or immunotherapy for example.
In the current radiation oncology paradigm, the evolution and development of novel, sophisticated technologies, which integrate volumetric imaging functionality with precise and accurate radiation delivery in real time, have allowed us to not only precisely target the radiation treatment to the patient-specific size, shape and location of the tumour, but have also allowed us to adapt the radiation treatment in real-time based on anatomical and functional changes which occur during the course of treatment, resulting in a truly personalized treatment for the patient.
While PCM in the context of radiation oncology takes on many different forms in each of our centres, it is guiding the most advanced clinical research and the redefining the future of radiotherapy practice.
Following are two examples of how PCM is being applied in the clinical setting.
Personalized Cancer Medicine using RaySearch's RayStation at the Princess Margaret Cancer Centre
By Tim Craig
Radiation medicine requires advanced software to review images, define tumours, and design personalized treatment plans for each patient. The Radiation Medicine Program at Princess Margaret is undergoing a massive technology change that will migrate external beam treatment planning to RaySearch’s RayStation treatment planning system. RayStation is an innovative system with novel features such as deformable image registration, dose accumulation, adaptive replanning, and proton planning. In fact, it contains several technologies that were developed within UTDRO, including the Morfeus deformable image registration algorithm and automated breast planning, developed by Tom Purdie, Kristy Brock, Michael Sharpe, and David Jaffray.
The decision to implement RayStation came from our strengths. A decade ago, UTDRO led the world in the implementation of image-guided radiation therapy (IGRT). This involves imaging and shifting the patient to correct for positioning errors immediately prior to irradiation. IGRT led to incredible improvements in treatment accuracy, and is now considered standard of care in highly conformal treatments. The value in these images however, are not being fully realized. They show that patients experience various anatomical changes, such as weight loss or tumour shrinkage, that lead to the delivered dose differing from the planned dose. Combining these images with algorithms for deformable image registration and dose accumulation, they can be used to monitor the dose delivered on a daily basis. This allows the exploration of the next frontiers in radiation medicine; RayStation was the first system to provide this opportunity.
Quantifying the dose delivered during treatment can identify the need to intervene, adapt, and replan a patient’s treatment. This is a form of treatment personalization known as adaptive radiation therapy (ART). The Princess Margaret Radiation Medicine Program has a strong interest in designing and evaluating innovative ART. UTDRO faculty, including Peter Chung, Charles Catton, and Tim Craig, have been successful in securing grants to conduct feasibility studies. Although the value of ART has been acknowledged for some time, large-scale implementation has been slow and difficult due to a lack of supporting systems. The RayStation platform positions UTDRO to accelerate the pace of ART.
Due to our strong research reputation, RaySearch was eager to collaborate. This research relationship has already yielded several publications by Michael Milosevic, Valerie Kelly, Young-bin Cho, Anthony Fyles, and David Jaffray on the potential for ART in cervical cancer, and prestigious plenary presentations at the American Society for Therapeutic Radiology and Oncology annual meeting by Michael Sharpe, Laura Dawson, and Brian O’Sullivan.
The potential for the combination of the RayStation platform with our expertise is recognized beyond the university. For example, UTDRO captured an impressive six of eight nationally available AbbVie – CARO and SANOFI-CARO grants this year. Four of these five were awarded for projects that directly use RayStation in their research (UTDRO Principal Investigator faculty included Vickie Kong and Michael Velec, and Fellows Michael Jones and Aravindhan Sundaramurthy).
In addition to enabling ART, dose accumulation may have other impacts on radiation oncology. UTDRO faculty David Jaffray and Patricia Lindsay outlined a vision in the highly cited QUANTEC publications with the hypothesis that dose accumulation leads to a better understanding of the dose actually delivered, which in turn leads to a better understanding of the relationship between dose and tumour control or toxicity. A UTDRO publication on this topic including Laura Dawson, Michael Velec, Jim Brierley, Rebecca Wong, and John Kim has provided preliminary validation of this hypothesis for tumour control in liver cancers.
In addition to our current implementation, our relationship with RaySearch has been deepened through their generous donation to create a Michael Sharpe Treatment Planning Learning Facility to support treatment planning education in the Medical Radiation Sciences Program, jointly run by the Michener Institute at University Health Network and UTDRO. This ensures that radiation therapy students in this program will have access to state of the art planning tools, and can graduate prepared for the most technologically advanced radiation treatments.
RayStation is a platform that enables the ambition within UTDRO. We look forward to using it as a foundation for delivering the most innovative clinical treatments, supporting the department’s future role as a leader in ART, and educating the next generation of radiation medicine professionals.
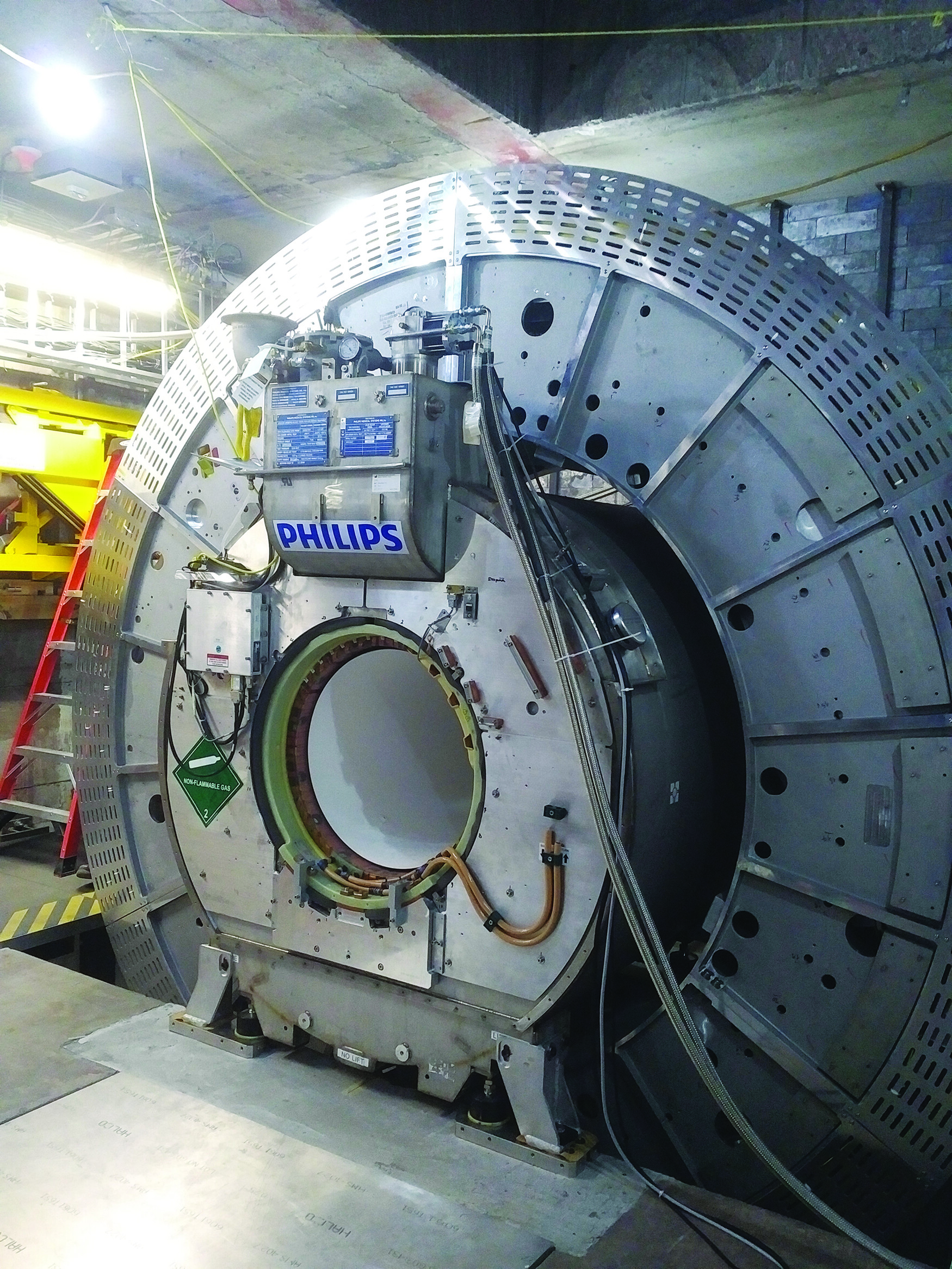
The MR-Linac for Adaptive and Personalized Radiotherapy at the Odette Cancer Centre
By Arjun Sahgal and Brian Keller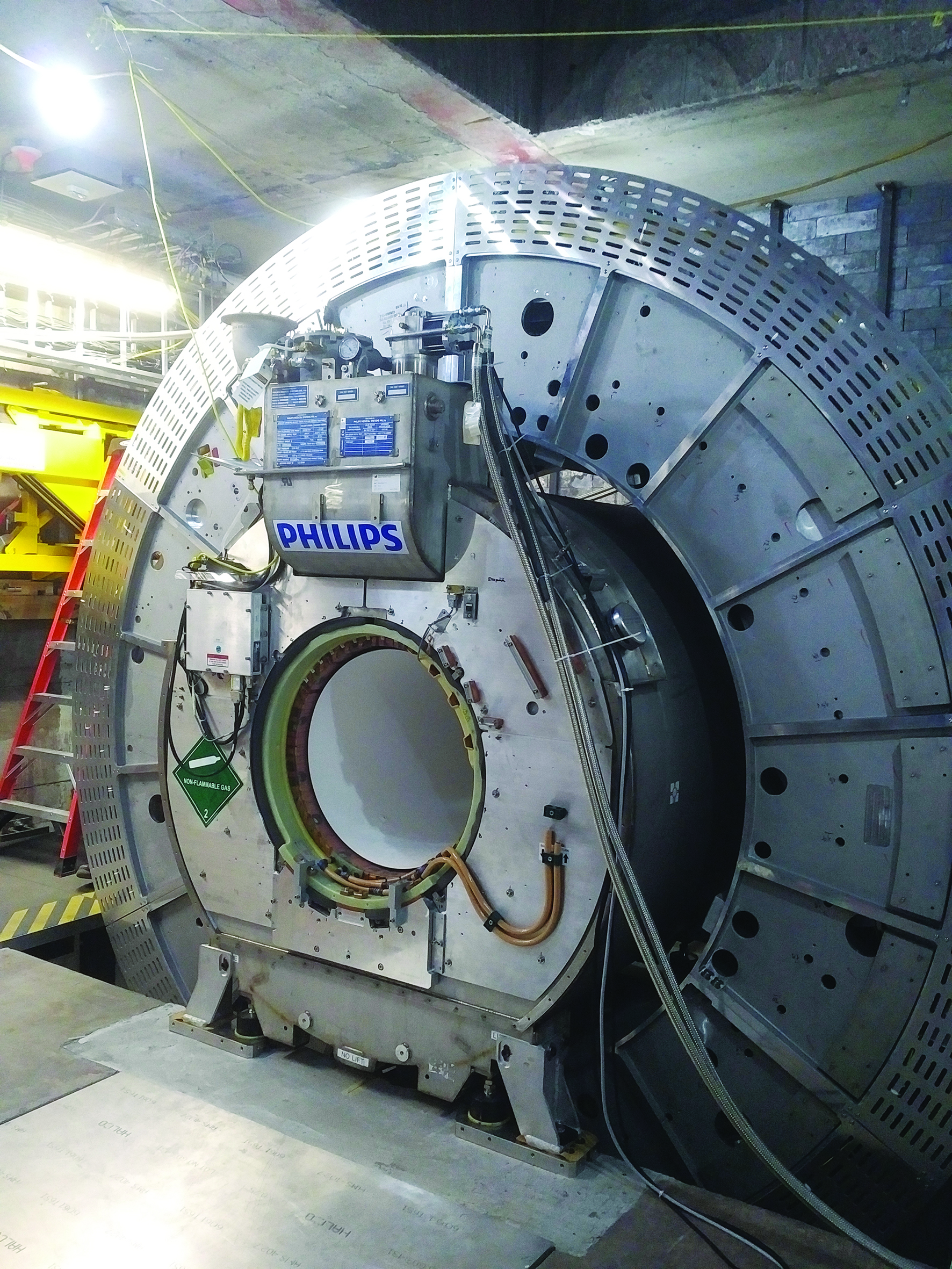
The development and clinical implementation of cone beam CT in the early 2000’s had a substantial impact on reducing geometric uncertainty; allowing for more conformal radiotherapy and the onset of image-guided radiotherapy (IGRT). This also paved the way for more ablative radiotherapy since target localization was improved. This is particularly exemplified in lung SBRT where a soft tissue tumour in the lung is readily visualized on CBCT.
In most other instances however, tumours and critical structures are not visible on CBCT, so one needs to rely on bony landmarks. Additionally, there is currently no real time tumour imaging during radiotherapy to allow for monitoring of beam-on tumour intrafractional motions/response.
The development of a hybrid, high field strength, integrated MRI-Linac system has the potential to fill some of these gaps, and to provide quantitative response assessment imaging with no imaging-related radiation dose.
At Sunnybrook, the first Canadian MRI-Linac has been installed, and as a member of a global consortium, we are currently evaluating this technology in a systematic fashion.
We will first apply this technology to brain tumor patients, evaluating daily changes to target volumes based on MRI, and use of functional imaging to assess treatment response. In addition, we will treat rectal, pancreas, and cervix patients as examples of our priority sites.
The proper tools are being implemented to allow for auto-segmentation of daily MR images, re-optimization of treatment plans in the presence of the magnetic field, and patient specific QA prior to daily modifications to treatments.
It is hypothesized that adaptation during radiotherapy, accounting for organs at risk (OAR), and target locations and deformations, would allow dose escalation and/or reduced side effects; yet this can only be answered in a number of well controlled clinical trials being organized through the Elekta MRI-Linac Consortium.
Image Credit: Tim Craig, Claire McCann